are diabetic foot wound cultures useful
What is DFU infection?
limb amputations are preceded by a Diabetic Foot Ulcer (DFU). A foot ulcer is a break of the skin of the foot to at least the level of the dermis that may result from trauma, neuropathy, ischemia and/or infection.
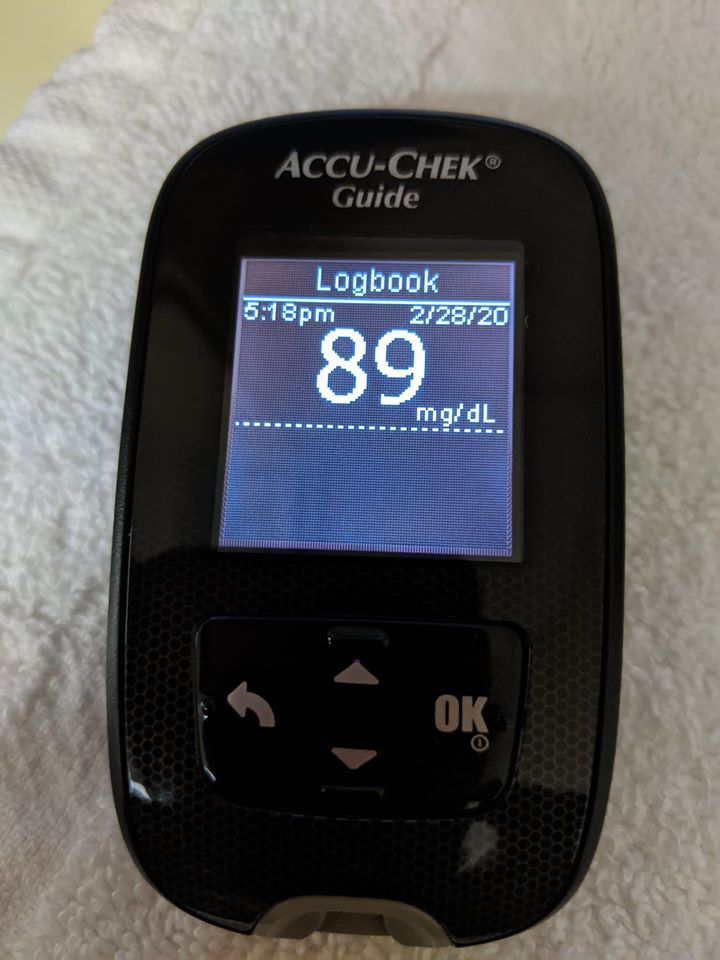
Thousands of people suffering from erratic blood sugar has been using this ground-breaking solution…
To help them burn away dangerous fat from their vital organs and bellies…
While stabilizing their blood sugar levels naturally and effectively.
And starting today…
What are the most common microorganism that present in an infected diabetic foot?
Diabetic foot infections are classified as mild, moderate, or severe. Gram-positive bacteria, such as Staphylococcus aureus and beta-hemolytic streptococci, are the most common pathogens in previously untreated mild and moderate infection.
Why are foot injuries bad for diabetics?
Over time, diabetes may cause nerve damage, also called diabetic neuropathy, that can cause tingling and pain, and can make you lose feeling in your feet. When you lose feeling in your feet, you may not feel a pebble inside your sock or a blister on your foot, which can lead to cuts and sores.
Can diabetic foot infection be cured?
Diabetic foot infections are a frequent clinical problem. About 50% of patients with diabetic foot infections who have foot amputations die within five years. Properly managed most can be cured, but many patients needlessly undergo amputations because of improper diagnostic and therapeutic approaches.
What does a diabetic foot infection look like?
Infections can cause constant pain, redness around an ulcer, warmth and swelling, pus, or an ulcer that does not heal. You should see your doctor as soon as possible if you have any of these signs.
Is there a link between diabetes and cellulitis?
Diabetics were significantly more likely than nondiabetics to have cellulitis as the presenting infection (67% of cases vs 56%, P=0.008) and to have lower extremity involvement (48% vs 33%, P<0.001) (Table 1).
What bacteria causes diabetic foot ulcer?
Diabetics with ulcers commonly experience infection with gram-positive organisms such as Staphylococcus aureus, Enterococcus, and gram-negative organisms like Pseudomonas aeruginosa, Escherichia coli, Klebsiella species, Proteus species, etc., and anaerobes. These organisms also show multi-drug resistance.
How do you treat a diabetic foot wound?
Keep the wound covered and moist For proper wound care, clean the wound with saline, apply a topical gel or antibiotic ointment medication to the wound once a day, as recommended by your doctor. After each application, wrap the wound with a clean gauze dressing.
Do you stage diabetic foot ulcers?
When treating diabetic foot ulcers it is important to be aware of the natural history of the diabetic foot, which can be divided into five stages: stage 1, a normal foot; stage 2, a high risk foot; stage 3, an ulcerated foot; stage 4, an infected foot; and stage 5, a necrotic foot.
Why can’t diabetics soak their feet?
Do not soak feet, or you’ll risk infection if the skin begins to break down. And if you have nerve damage, take care with water temperature. You risk burning your skin if you can’t feel that the water is too hot.
Why can’t diabetics cut toenails?
Diabetes may cause nerve damage and numbness in your feet, which means you could have a foot wound without knowing it. Poor circulation makes healing harder, which increases your risk of infection and slow-healing wounds.
What is the number one complication of diabetics?
Nerve damage (neuropathy): One of the most common diabetes complications, nerve damage can cause numbness and pain. Nerve damage most often affects the feet and legs but can also affect your digestion, blood vessels, and heart.
Will diabetic foot ulcers ever heal?
People with diabetes and lower extremity arterial disease often heal slowly, so it may take weeks or months for a foot ulcer to heal completely.
How do you debride a diabetic foot ulcer?
This technique utilises a surgical instrument, such as a scalpel, curette, or tissue nipper to remove devitalised tissue. Its advantage is that it is selective, removing mainly non-vital tissue. Optimal use of surgical debridement requires a very skilled clinician to avoid damage to healthy surrounding tissue.
Why do foot ulcers occur in diabetic patients?
How Do Diabetic Foot Ulcers Form? Ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes.
Should diabetics wear socks to bed?
Consider socks made specifically for patients living with diabetes. These socks have extra cushioning, do not have elastic tops, are higher than the ankle and are made from fibers that wick moisture away from the skin. Wear socks to bed. If your feet get cold at night, wear socks.
Which ointment is best for diabetic wound?
Antibiotics such as Neomycin, Gentamycin, and Mupirocin have good antibacterial coverage when used topically. Silver containing dressings come in different formulations and have very good antibacterial coverage. Silver dressings and polyherbal preparations have shown good results in healing diabetic foot wounds[74].
When should a diabetic foot be amputated?
Wounds need to be monitored frequently, at least every one to four weeks. When the condition results in a severe loss of tissue or a life-threatening infection, an amputation may be the only option. A surgeon will remove the damaged tissue and preserve as much healthy tissue as possible.
How do you classify a diabetic foot ulcer and infection?
These include: grade 0 (intact skin), grade 1 (superficial ulcer), grade 2 (deep ulcer to tendon, bone, or joint), grade 3 (deep ulcer with abscess or osteomyelitis), grade 4 (forefoot gangrene), and grade 5 (whole foot gangrene).
How do you describe a diabetic foot ulcer?
A diabetic foot ulcer is a skin sore with full thickness skin loss often preceded by a haemorrhagic subepidermal blister. The ulcer typically develops within a callosity on a pressure site, with a circular punched out appearance. It is often painless, leading to a delay in presentation to a health professional.
My successful Diabetes Treatment Story
My doctor diagnosed me with diabetes just over a year ago, at the time I was prescribed Metformin. I went to the some diabetes related websites and learned about the diet they suggested. I started the diet right away and I was very loyal to it. However, after weeks of being on the diet it never helped, my blood sugar didn’t drop like I wanted it to. My personal physician wasn’t much help either, he didn’t really seem to give me any other options besides my prescription and the usual course of insulin. I was about to give up and then I discovered a great treatment method. The guide was authored by one of the leading professionals in the world of diabetes research, Dr. Max Sidorov. This is a guide that that shows you, in a very simple way, how to conquer the disease without traditional methods. I have to say that since I’ve found the guide and followed it, I’ve not only improved my health but I’ve also lost weight and improved other aspects as well. My activities have increased and I have a ton of energy! It is my goal to share the this diabetes treatment method as much as possible to show people there’s more to the disease than traditional schools of thought and you can find your own path to healing with natural methods.Thousands of people suffering from erratic blood sugar has been using this ground-breaking solution…
To help them burn away dangerous fat from their vital organs and bellies…
While stabilizing their blood sugar levels naturally and effectively.
And starting today…
